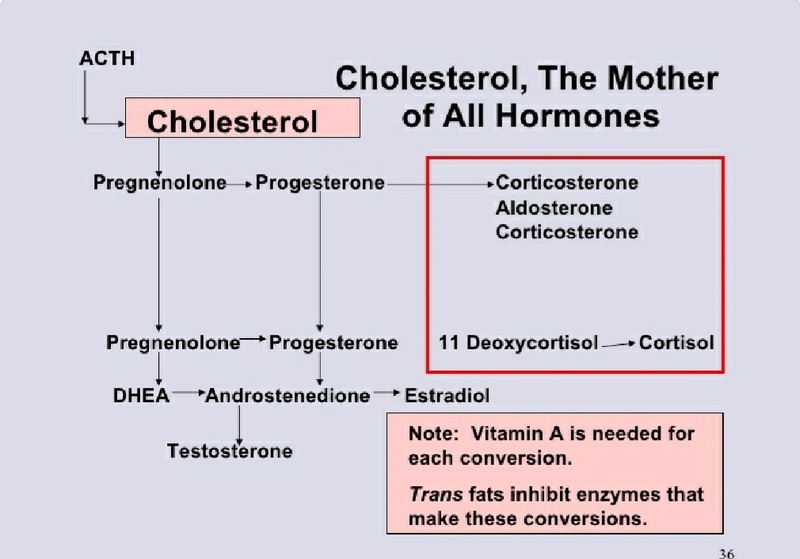
Cholesterol is an essential molecule without which there would be no life, so important that virtually every cell in the body is capable of synthesizing it. Among its other duties, cholesterol is a major structural molecule, a framework on which other critical substances are made. Were we able to somehow remove all its cholesterol, the body, would, in the words of Shakespeare, “melt, thaw and resolve itself into a dew.” And that’s not to mention that we wouldn’t have bile acids, vitamin D, or steroid hormones (including sex hormones), all of which are cholesterol-based.
Cholesterol plays a big role in helping fight bacteria and infections. A study that included 100,000 healthy participants in San Francisco over a fifteen-year period found that those with low cholesterol values were much more likely to be admitted to hospitals with infectious diseases.
Sixty years ago a researcher, little known outside of academic circles, singlehandedly set us on this path of cholesterol paranoia: Ancel Keys, Ph.D., a proponent of what has become known as the lipid hypothesis, concluded that excess cholesterol caused heart disease. He started out thinking that dietary fat in general drove cholesterol levels up, but as the years went by, he came to believe that saturated fat was the true cholesterol-raising villain. (This idea of saturated fat as villain is so ingrained in the minds of health writers that the words “saturated fat” are almost never written alone but always as “artery-clogging saturated fat.”) Which is more or less the basis for the lipid hypothesis: saturated fat runs up cholesterol levels, and elevated cholesterol leads to heart disease.
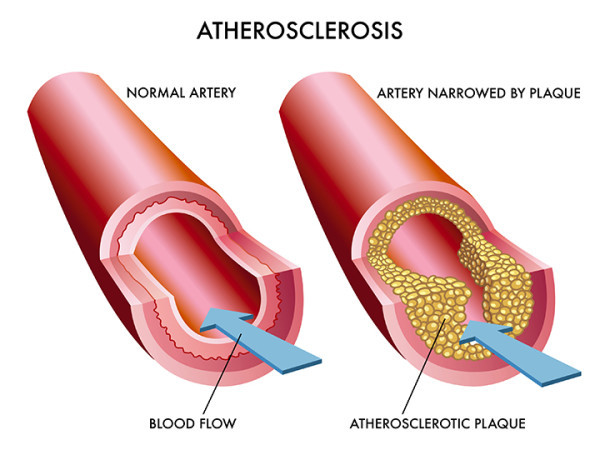
Nice and simple, but not true. It has never been proven, which is why it is still called the lipid hypothesis. Because of Keys’s influence, researchers for the past five decades have been beavering away in labs the world over, desperate to find enough actual proof to convert the lipid hypothesis into the lipid fact. But so far, they’ve fallen way short. In the process, however, they have vastly expanded our knowledge of the biochemistry and physiology of the cholesterol molecule. Thanks to their efforts, we now know that cholesterol is transported in the blood attached to carrier proteins, and that these protein-cholesterol complexes are called lipoproteins. Their densities now describe these lipoproteins: HDL (high-density lipoprotein), LDL (low-density lipoprotein), VLDL (very-low-density lipoprotein), and a number of others. Some of these lipoproteins are considered good (HDL) and others bad (LDL). And, of course, the drug companies have developed medications purported to increase the former while decreasing the latter.
Researchers have discovered a type of lipoprotein called small, dense (or type B) LDL that may actually end up being a true risk factor for heart disease. Problem is, this small, dense type B LDL is worsened by the very diet those promoting the lipid hypothesis have hailed for decades as the best diet to prevent heart disease: the low-fat, high-carbohydrate diet. Turns out that fat, especially saturated fat, decreases the amount of these small, dense LDL particles while the widely recommended low-fat diet increases their number. The opposite of the small dense LDL are large fluffy (or Type A) LDL particles, which are not only not harmful but are actually healthful. But the LDL–lowering drugs lower those, too.
Cracks should have appeared in the firm entrenchment of the lipid hypothesis (that now basically posits that elevated LDL causes heart disease) when a recent study showed that of almost 140,000 patients admitted to the hospital for heart disease, almost half of them had LDL levels under 100 mg/dL (100 mg/dL has been the therapeutic target for LDL for the past few years). Instead of stepping back, scratching their heads, and thinking, Hmmm, maybe we’re on the wrong track here, the authors of this study concluded that maybe a therapeutic level of 100 mg/dL for LDL is still too high and needs to be even lower. Such is their lipo-phobic herd mentality.
The millions of marketing dollars spent on perpetuating this myth have successfully kept us focused on a relatively minor character in the heart disease story, and created a market for cholesterol-lowering drugs worth more than $30 billion a year. The real tragedy is that by putting all of our attention on cholesterol, we’ve virtually ignored the real causes of heart disease:
Inflammation, Oxidation, Sugar and Stress.
When the National Cholesterol Education Program lowered the “optimal” cholesterol levels in 2004, eight out of nine people on the panel had financial ties to the pharmaceutical industry.
• Cholesterol is a minor player in heart disease.
• Cholesterol levels are a poor predictor of heart attacks.
• Half the people with heart disease have normal cholesterol.
• Half the people with elevated cholesterol have healthy hearts.
• Lowering cholesterol has extremely limited benefits.
We were consuming whole, full-fat foods such as cream, butter, pasture-raised meats, raw milk, and other traditional foods, the rate of heart disease was a fraction of what it is now. I wonder whether it is indeed a coincidence that the twin global pandemics of obesity and diabetes just happened to occur around the time we collectively banished these foods because of the phobia about cholesterol and saturated fat in the diet and began to replace them with vegetable oils, processed carbs, and, ultimately, trans fats.
Now comes the question of cholesterol rich foods increasing cholesterol in the body.

Our liver produces anywhere from 1-2 grams of cholesterol per day. Vital learning: The production can decrease when we eat cholesterol-rich foods and increase when we eat foods without cholesterol. That means your liver adapts to your alimentary cholesterol intake, or in other words, your liver regulates the cholesterol in your bloodstream. This is why you see normalized or even high cholesterol levels among vegetarians.
- Coenzyme Q10 (CoQ10), an absolutely vital nutrient that is made in every cell in the body and is a major chemical participant in the production of cellular energy. CoQ10 is critically important for the strong pumping action of the heart, which gobbles the stuff up. Recently I discovered something that shook my belief in statin drugs to the core—they depleted the body of CoQ. This fact was to be added as a warning on statin cartons and inserts but the FDA (Food and Drug Administration) decided against it in 2014. How ironic that the very drug they prescribe to reduce the likelihood of a heart attack actually deprives the heart of the fuel it needs to perform properly? No wonder fatigue, low energy, and muscle pain are such frequent accompaniments to statin drug use.
- Vitamin K2 which protect the arteries from calcium buildup is inhibited by statins. This is significant because K2, along with magnesium (Mg) is vital in moving calcium out of the soft tissues and into the bones where it belongs.
- Mitochondrial dysfunction. Our energy is produced in the mitochondria and statins are toxic to these energy centres in our cells, disrupting ATP (adenosine triphosphate) production, which is our energy currency. This in turn compromises heart muscle function and disrupts intracellular signals.
- Statins and Ketones. Dr. Aseem Malhotra, an interventional cardiologist consultant in London, U.K. says that statins block the formation of ketones. Ketones are an essential part of mitochondrial nutrition and overall health. If you can’t make ketones, you impair the metabolism in your entire body. This includes your heart which raises your risk for heart disease and a variety of other conditions.
- Selenium-containing proteins: Statins interfere with Selenoproteins such as glutathione peroxidase. These proteins are vital in preventing oxidative damage to muscle tissue.
Watch the video that shows studies which says chances of heart disease did not decrease despite the low cholesterol levels.
The Lyon Diet Heart Study found that certain dietary and lifestyle changes were able to reduce deaths by 70 percent and reduce cardiovascular deaths by an even more impressive 76 percent, all without making as much as a dent in cholesterol levels.
The Nurses’ Health Study2 found that 82 percent of coronary events were attributable to five factors, none of which had anything to do with lowering cholesterol.